Neurological and Stroke Care
Visit the Neuroscience Institute at Christ Hospital website at https://neuroscience-institute.carepointhealth.org to learn more.
Neurology is a broad field because our nervous system spans our entire body. That’s why our team works closely with each individual’s primary care physician and other multidisciplinary specialists to provide the most effective treatment and achieve the best possible outcomes for conditions affecting the brain, spine and nervous system.
The New Jersey Department of Health and Senior Services has certified our three hospitals—Bayonne Medical Center, Christ Hospital and Hoboken University Medical Center—as Primary Stroke Centers.
Stroke Treatments
In stroke, “time is brain.” Stroke is an emergency where getting the right care, right away is critical to both life and quality of life. We are able to treat ischemic and hemorrhagic stroke, as well as transient ischemic attacks known as a mini stroke.
Stroke Rehabilitation
Steps taken after a stroke can help achieve the best possible recovery. Many of the effects of stroke are treatable during recovery. In fact, the first two weeks after a stroke are the most important opportunity for rehab efforts and can yield the most gain.
Telestroke
No matter when someone suffering a stroke arrives at the hospital, they are guaranteed to be seen by a stroke certified neurologist within minutes. This service allows them to receive the appropriate treatment as soon as possible.
Epilepsy Monitoring Unit
Our unit makes diagnosing and monitoring seizures easier on patients through routine and ambulatory EEG monitoring—giving individuals and their neurologists a better understanding of what’s happening.
Christ Hospital Stroke Patient Outcomes
The American Heart Association Get With The Guidelines-Stroke Award
CarePoint Health – Christ Hospital has received the American Heart Association’s Get With The Guidelines® Stroke Gold Plus with Target: Stroke Honor Roll with Target: Type 2 Diabetes Honor Roll. Award for our commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines.
Hospitals receiving Get With The Guidelines® Gold Plus Achievement Award have reached an aggressive goal of treating patients with 85 percent or higher compliance to core standard levels of care as outlined by the American Heart Association/American Stroke Association® for 2 consecutive calendar years. In addition, those hospitals have demonstrated 75 percent compliance during the 12-month period.
Our multidisciplinary team of specialists from neurology, neurosurgery, neuro-intensive care, neuro-interventional, neuroscience nursing, emergency medicine work together to care for patients with the most complex medical and surgical conditions and get them on the road to recovery.
Community Prevention and Education
Risk Factors for Stroke
To prevent stroke, know your risk factors and have regular medical checkups.
Some risk factors can be changed and some cannot.
High blood pressure is the single most important risk factor for stroke because it’s the No. 1 cause of stroke. If your blood pressure is consistently 140/90 or above, it’s high. Have it checked by your doctor at least once every two years and talk to your doctor about how to manage it.
- Tobacco use damages blood vessels. Don’t smoke, and avoid second-hand smoke.
- Diabetes mellitus. Having diabetes increases your risk of stroke because it can cause disease of blood vessels in the brain. Work with your doctor to manage diabetes.
- High blood cholesterol increases the risk of blocked arteries. If an artery leading to the brain becomes blocked, a stroke can result.
- Physical inactivity and obesity. Being inactive, obese, or both, can increase your risk of cardiovascular disease.
- Carotid or other artery disease. The carotid arteries in your neck supply most of the blood to your brain. A carotid artery damaged by a fatty buildup of plaque inside the artery wall may become blocked by a blood clot, causing a stroke.
- Transient ischemic attacks (TIAs). Recognizing and treating TIAs can reduce the risk of a major stroke. TIAs produce stroke-like symptoms but have no lasting effects. Know the warning signs of a TIA and seek emergency medical treatment immediately.
- Atrial fibrillation or other heart disease. In atrial fibrillation the heart’s upper chambers quiver rather than beating effectively. This causes the blood to pool and clot, increasing the risk of stroke. People with other types of heart disease have a higher risk of stroke, too.
- Certain blood disorders. A high red blood cell count makes clots more likely, raising the risk of stroke. Sickle cell anemia increases stroke risk because the “sickled” cells stick to blood vessel walls and may block arteries.
- Excessive alcohol intake. Drinking an average of more than one drink per day for women or more than two drinks a day for men raises blood pressure. Binge drinking can lead to stroke.
- Illegal drug use. Intravenous drug use carries a high stroke risk. Cocaine use also has been linked to stroke. Illegal drugs commonly cause hemorrhagic strokes.
- Increasing age. Stroke affects people of all ages. But the older you are, the greater your stroke risk.
- Gender. In most age groups, more men than women have stroke, but more women die from stroke.
- Heredity and race. People whose close blood relations have had a stroke have a higher risk of stroke. African Americans have a higher risk of death and disability from stroke than Caucasians, because they have high blood pressure more often. Hispanic Americans are also at higher risk of stroke.
- Prior stroke. Someone who has had a stroke is at higher risk of having another one.
When a Stroke Occurs:
Rapid Stroke Treatment Can Save Lives
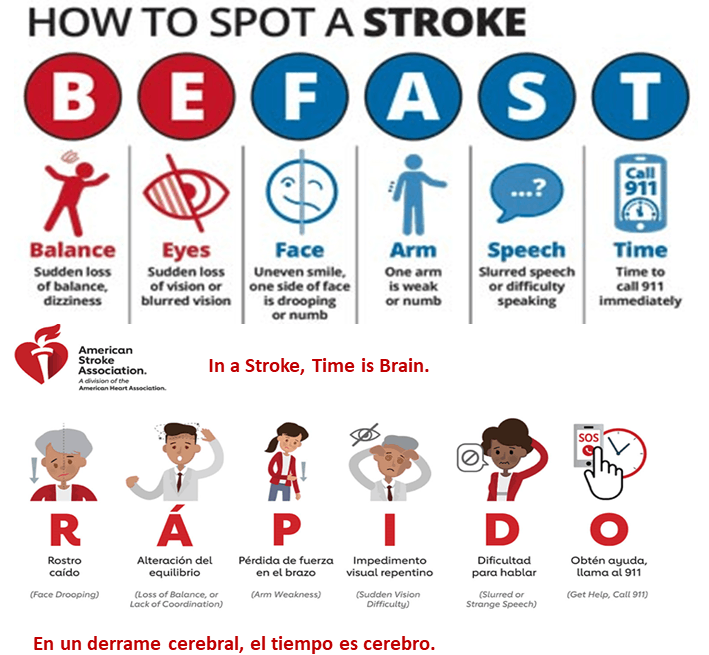
If you’re having a stroke, it’s critical that you get medical attention right away. Immediate treatment may minimize the long-term effects of a stroke and prevent death.
There are two types of strokes: hemorrhagic or ischemic.
An ischemic stroke occurs as a result of an obstruction within a blood vessel supplying blood to the brain. It accounts for 87 percent of all stroke cases.
A hemorrhagic stroke occurs when a weakened blood vessel ruptures and spills blood into brain tissue. The most common cause for the rupture is uncontrolled hypertension (high blood pressure).
There are two other types of weakened blood vessels that also cause hemorrhagic stroke: aneurysms and AVMs. Treatment differs depending on the type of stroke.
- Brain edema — swelling of the brain after a stroke.
- Pneumonia — causes breathing problems, a complication of many major illnesses.
- Common swallowing problems after stroke can sometimes result in things “going down the wrong pipe”, leading to aspiration pneumonia.
- Urinary tract infection and/or bladder control.
- Seizures — abnormal electrical activity in the brain causing convulsions.
- Clinical depression — a treatable illness that often occurs with stroke and causes unwanted emotional and physical reactions to changes and losses.
- Bedsores — pressure ulcers that result from decreased ability to move and pressure on areas of the body because of immobility.
- Limb contractures — shortened muscles in an arm or leg from reduced range of motion or lack of exercise.
- Shoulder pain — stems from lack of support of an arm due to weakness or paralysis. This usually is caused when the affected arm hangs resulting in pulling of the arm on the shoulder.
- Deep venous thrombosis — blood clots form in veins of the legs because of immobility from stroke.
Related Resources
- American Stroke Association
- Resource Library
Clinical Practice Guidelines:
- Stroke Training for EMS Professionals